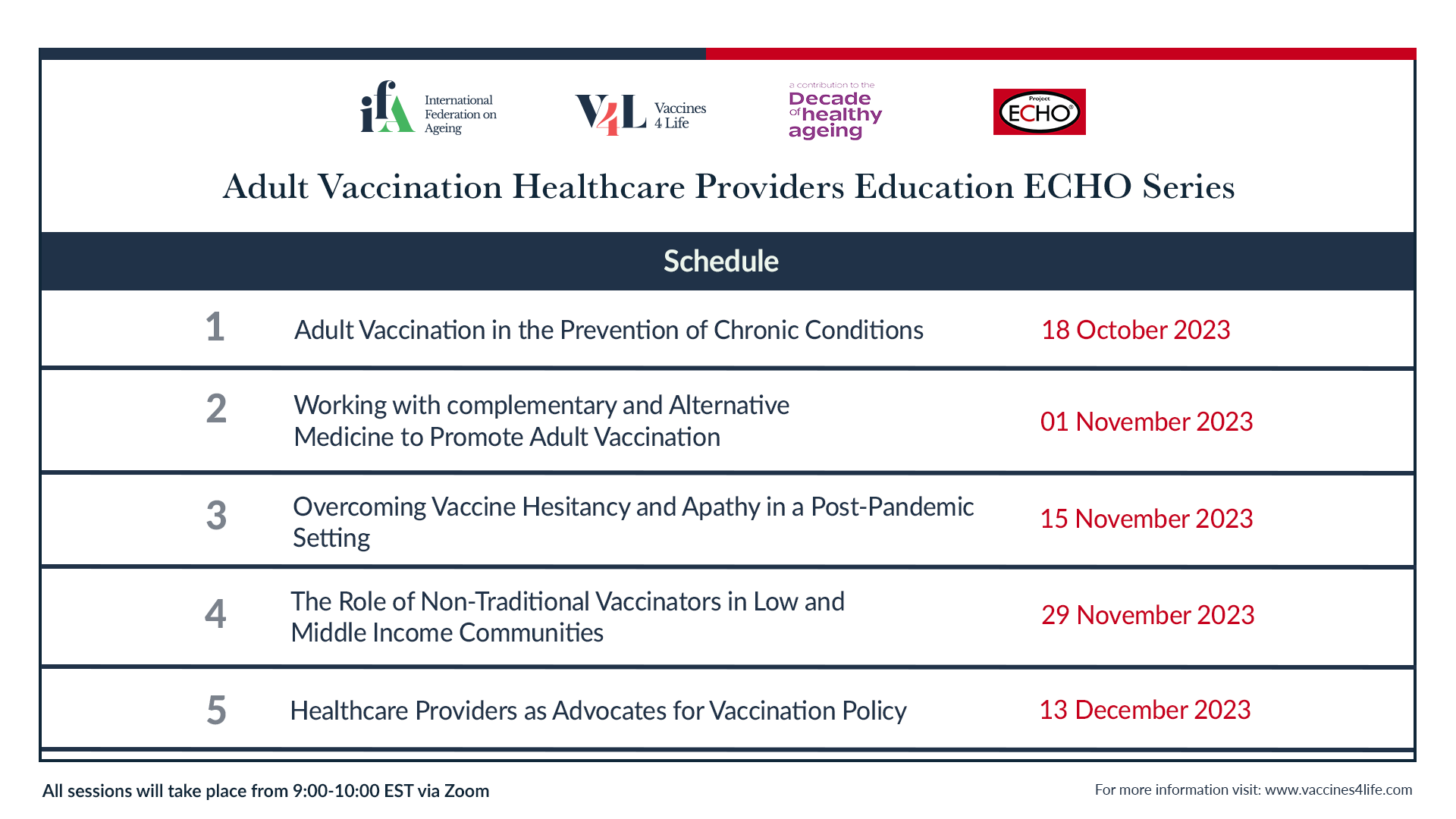
Adult Vaccination Healthcare Providers Education ECHO Series

The recent AV-HCP ECHO program has proven successful in improving knowledge, skills, and capacity of HCPs that work within the field of healthy ageing. The technical report on this series details its purpose and impact and provides key recommendations, which can help guide HCPs around the world in improving their advocacy work and adult vaccination rates through their practices. Sessional resources developed from the modules have also been included here to supplement adult immunization advocacy knowledge for HCPs.
AV-HCP ECHO Program Sessional Resources
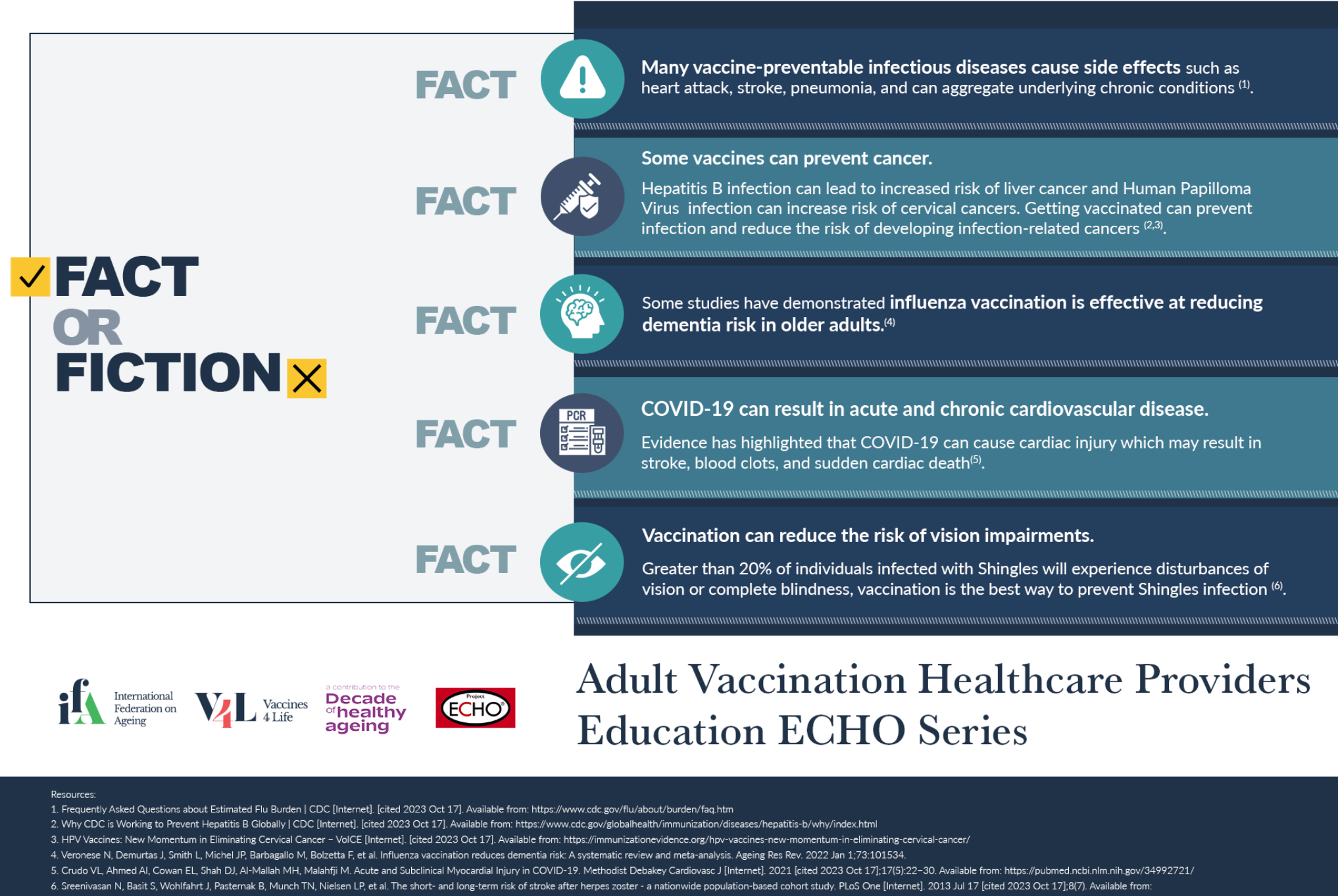
Module 1: Adult vaccination in the prevention of chronic conditions
Click on the images below to download the assets for Module 1.
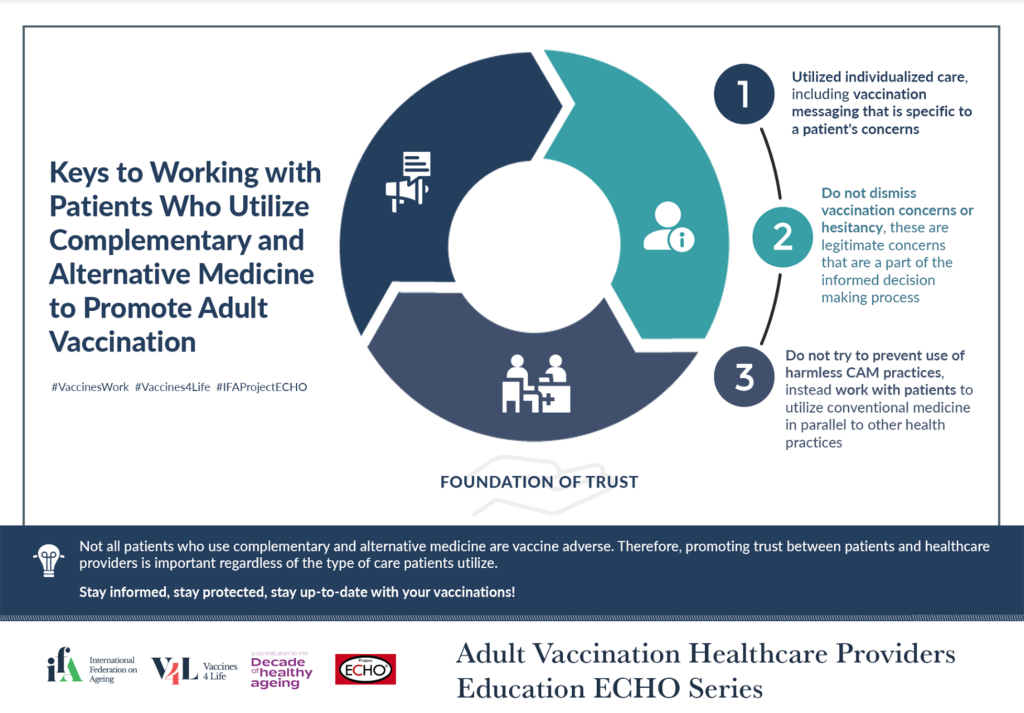
Module 2: Collaborating with Complementary and Alternative Medicines to promote adult vaccination
Click on the images below to download the assets for Module 2.
Module 3: Overcoming vaccine hesitancy in a post-pandemic setting
Click on the images below to download the assets for Module 3.
Module 4: The Role of Non-Traditional Vaccinators in Low- and Middle-Income Environments
Click on the images below to download the assets for Module 4.
Module 5: Healthcare Providers as Advocates for Vaccination Policy
Click on the images below to download the assets for Module 5.
Anatomy of an ECHO
The ECHO ModelTM has been leveraged across many fields including education and social justice. There are more than 860 ECHO networks in 44 countries that have trained more than 148,000 learners from 30,000 organizations. Project ECHO is a hub-and-spoke model which connects organizations (the “spokes”) with a group of experts (the “hub”). Each learning session involves a didactic component, or lecture, from subject matter experts followed by case presentations from learners to facilitate practice, mastering complexity and sharing best practices. Participants learn from one another, as knowledge is tested and refined through a local lens.
This continuous loop of learning, mentoring and peer support is what makes the AV-HCP ECHO unique, with a long-lasting impact far beyond that of a webinar or an e-learning course.
| The Hub | The Spokes (learners) | Session facilitator | |
| Who? | Experts / thought leaders in the field of adult vaccination representing diverse healthcare professions | Healthcare providers looking to learn more about emerging adult vaccination topics | International federation on Ageing (IFA) representative |
|
Roles and Responsibilities
|
Subject matter experts:
|
If invited to present a case presentation:
If not presenting a case:
|
Session facilitator:
Synthesize learnings and key messages |
Media Toolkit
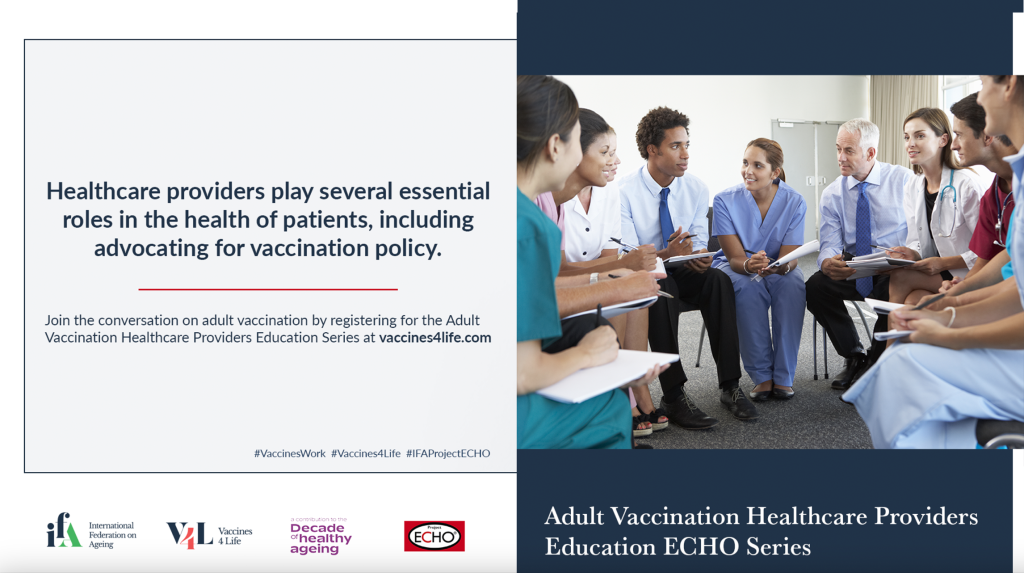
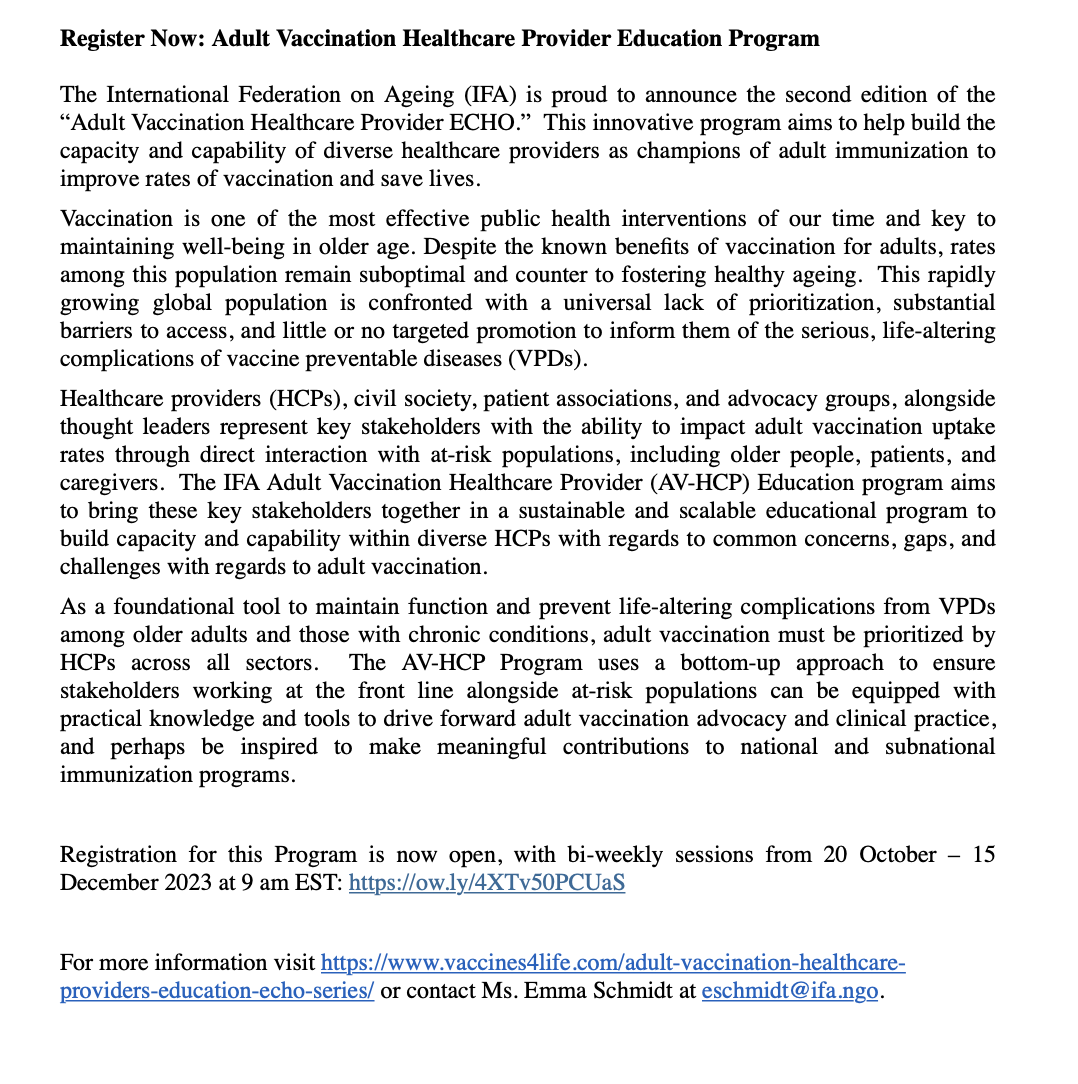
The IFA is pleased to be releasing an expanded session of the Adult Vaccination Healthcare Provider (AV-HCP) ECHO series. The series will occur bi-weekly from 18 October – 13 December 2023.
Against the backdrop of a global pandemic, there is an urgent need to health care professionals to be fully informed on the importance of adult immunization. The AV-HCP ECHO provides a safe learning environment to support this important virtual collaboration, as it brings together a community of multidisciplinary experts to crowdsource knowledge and curate solutions for improving adult vaccination rates. Moreover, the AV-HCP ECHO serves as a launching pad for the development of a global roadmap to apply learnings shared within the educational series to the global context.
Partnerships and collaborations give power and purpose to the work of improving the lives of older people and we would be grateful for your support in sharing information around this initiative throughout your extensive network.
We hope through the various options below organizations will be able to promote the ECHO series which aims to address current challenges and gaps in understanding experienced by healthcare providers globally. This is an excellent learning and sharing opportunity for current and future healthcare providers alike and will be made stronger through robust and diverse participation.
“The International Federation on Ageing (IFA) is proud to announce another instalment of the Adult Vaccination Healthcare Providers Education ECHO. The program – taking place biweekly from October 18-December 13 aims to strengthen healthcare provider skills and competencies to promote and advocate for adult immunization. Building on previous programming and experience, IFA will harness the ECHOTM Model and its proven method of learning for this innovative program to educate and inform diverse healthcare providers on the field of ageing and VPDs. The model allows for participatory dialogue and allows current and future healthcare providers the opportunity to seek recommendations directly from a panel of subject matter experts. For more information and to register, please visit the Vaccines for Life website.”
Click on the logos to download the high resolution version.
* If another variation and/or format of the logos is needed, please contact Ms. Berenice Anaya at banaya@ifa.ngo
Curriculum
Adult vaccination in the prevention of chronic conditions
While the value of vaccines in preventing infections of communicable viral diseases is often noted, additional benefits of vaccination include lowering the risk of certain chronic non-communicable diseases (NCDs). Vaccination against human papilloma virus, for example, can lower the risk of developing cervical cancer by as much as 87% and influenza vaccination can contribute to a 20-40% reduction of adverse cardiac events (1,2). When promoting healthy aging, preventing chronic diseases is a key objective, as NCDs are the leading cause of death globally.
Additionally, patients with co-morbidities are often more likely to have severe health outcomes in the event that they contract a vaccine preventable disease. Therefore, working with patients to highlight the value of adult vaccination as part of their own care plans is important regardless of the care provider they are working with. Vaccination can promote systemic health and prevent chronic conditions that impact all levels of human health, therefore encouraging vaccination should be the priority of all healthcare providers.
This module will explore the relationships between VPDs and NCDs, highlighting the value of integrating adult vaccination across disciplines and as a key component in ensuring a person-centered approach to healthy ageing.
Relevant Resources:
- Blindness: Converting the Vaccine Hesitant
- The Role of Noncommunicable Diseases in the Pursuit of Global Health Security
- Vaccination of Special-Risk Groups: A toolkit for pharmacists
Learning Objectives:
- Understand how co-morbidities of chronic and vaccine-preventable diseases as well as disability can lead to worsened health outcomes across the life course and for older adults.
- Discuss the benefits of vaccinations in maintaining systemic health through the prevention of chronic NCDs (i.e., HPV vaccine can prevent against cervical cancers, Hepatitis B vaccines can lower the risk of liver cancers).
- Highlight methods to reach at-risk populations of NCDs and VPDs.
Collaborating with Complementary and Alternative Medicines to promote adult vaccination
Complementary and Alternative Medicine (CAM) practices have been growing in popularity around the world and remain a dominant practice in many communities globally. CAM includes the use of homeopathy, acupuncture, massage, naturopathy, chiropractic care, and other practices. The use of CAM practices however is also associated with greater levels of vaccine hesitancy and reduced vaccination rates. However, CAM practices remain a culturally significant form of care for many patients globally and contribute to an individual’s right to choose the form of healthcare that they feel best suits their needs and they trust. Complementary medicine can also be used in conjunction with conventional medicine to provide a holistic and integrative approach to a person’s health and wellbeing.
There are many challenges to contextualizing the use and prevalence of CAM practices globally. Different definitions of CAM practices, and a lack of reporting and data collection relating to use of CAM contribute to the gaps in understanding how these practices are being used in different communities. However, systematic reviews have placed the use of CAM practices between 24-71.3% depending on the countries reviewed (3). This widespread use of some form of CAM practice shows the value of working with trusted CAM practitioners to promote vaccination as a strategy to improve vaccine uptake in a culturally specific and respectful way.
Additionally, there can be approaches to care within CAM practices that all HCPs can learn from. Despite misconceptions from many primary care providers, CAM practices are not inherently vaccine adverse, but instead focus on individualized care plans, understanding patient’s vaccine concerns and risks of VPDs, and taking vaccine concerns seriously (4). These practices can be adopted into all levels of healthcare to provide a patient centered approach.
Collaboration between CAM practitioners and HCPs can work to remove barriers, provide evidence informed recommendations, and align narratives around vaccination. This module explores good practices in multisectoral collaboration and fostering stronger connections as pathways for knowledge sharing between CAM practitioners and healthcare providers to respond to gaps in adult vaccination strategies, including during crisis settings.
Relevant Resources:
Collaborating with CAM Providers when Writing HPV Vaccine Review Articles
Naturopathic Medicine on the Frontline of the COVID-19 Pandemic
Learning Objectives:
- Understand the role of vaccination within complementary and alternative medicine practices.
- Discuss current and historical concerns that some CAM patients have had with vaccination.
- Provide HCPs and CAM practitioners with relevant communication and collaboration tools to improve vaccination rates.
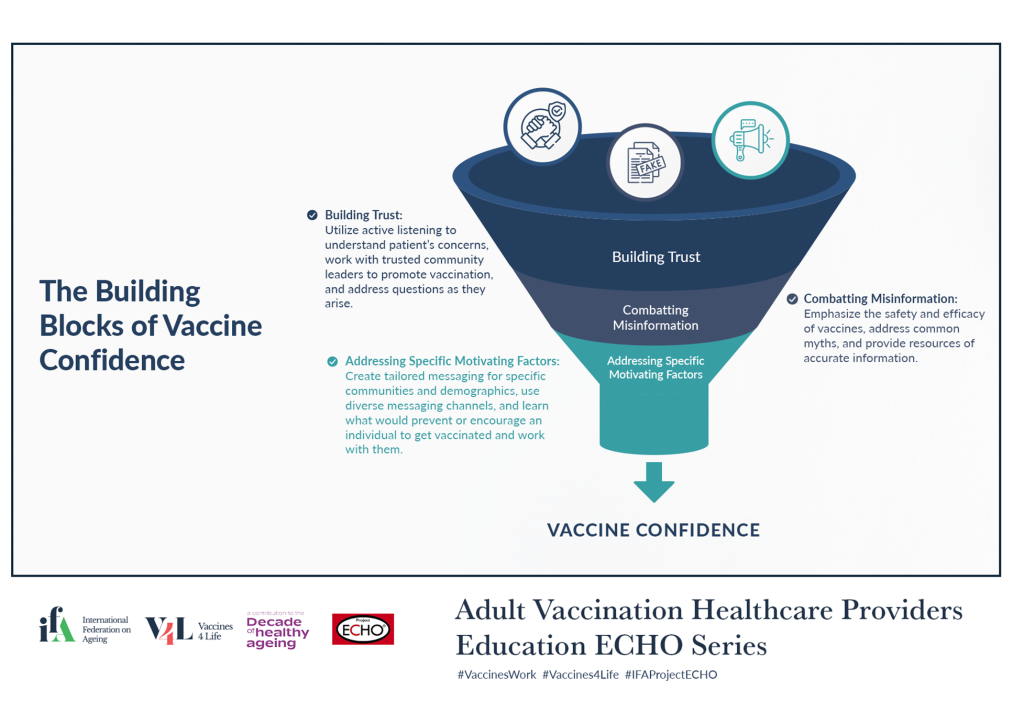
Overcoming vaccine hesitancy in a post-pandemic setting
The Covid-19 Pandemic brought about an increased urgency and focus on adult vaccination, including the prioritization of vaccination and vaccine campaigns for policy makers and healthcare providers. Despite the increased messaging, funding, and prioritization of adult vaccination, the Covid-19 pandemic also saw increases in vaccine hesitancy and misinformation. The quickly evolving nature of the novel disease brought with it rapidly changing health information and vaccine recommendations for individuals globally. With Covid-19 being declared endemic in Spring 2023, there is a new need to address patient concerns around endemic diseases and to continue to advocate for routine immunization and overcoming vaccine hesitancy despite a decreased threat to Covid-19.
During the Covid-19 pandemic, vaccine priorities became heavily focused on the COVID-19 vaccination. This prioritization, along with closures and difficulty accessing appointments at healthcare centers lead to vaccination for non-Covid-19 infections (such as influenza) declining (5). In a post-pandemic world, it is crucial to address these concerns and work with patients to “catch-up” on missed vaccines and overcome vaccine hesitancy and apathy for all vaccinations – not just for Covid-19. Vaccine apathy can be a particularly difficult barrier to address, as these individuals may view vaccination as a low-risk activity but not feel it is important to prioritize routine vaccination across the life course. Simplifying the pathways to receive vaccination is one way to prevent loss to follow-up due to vaccine apathy but use of messaging that addresses apathy and not just vaccine hesitancy is also critical.
This module works to address changes to vaccine perceptions that have occurred due to the Covid-19 Pandemic and how HCPs can address these changes following the latest updates to the status of Covid-19 and other VPDs.
Relevant Resources:
- Is Vaccine Confidence an Unexpected Victim of the COVID-19 Pandemic?
- Vaccine Hesitancy: Lessons Learned and Perspectives for a Post-Pandemic Tomorrow
- When Vaccine Apathy, Not Hesitancy, Drives Vaccine Disinterest
Learning Objectives:
- Understand how and why vaccine confidence and vaccine hesitancy rates have changed before and after the COVID-19 Pandemic, specifically for older adults.
- Discuss ways to improve vaccine confidence and vaccine promotion in a post-pandemic context including the use of co-administered vaccines.
- Learn how to cope with patient vaccine fatigue and apathy with health messaging and encourage routine immunization uptake for all recommended adult vaccine
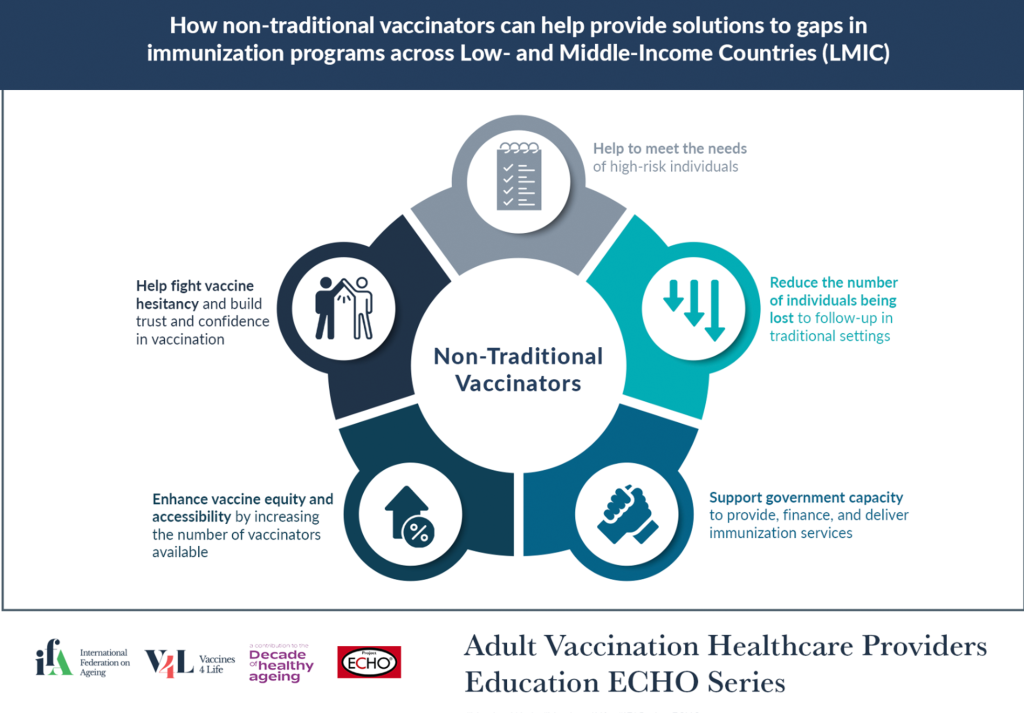
The role of non-traditional vaccinators in low- and middle- income environments
Working within low- and middle- income environments provide additional challenges and barriers for healthcare providers and their patients to overcome. Patients may have fewer resources available to access high-quality and timely information on vaccination, be limited in their ability to travel to vaccination appointments and have larger concerns with paying for vaccines that are not covered under private or public insurance schemes.
As healthcare providers, working with these individuals and communities is crucial to increasing vaccine rates in an equitable way that prioritizes the patients’ experiences. Using non-traditional vaccinators such as pharmacists, can work to reduce barriers to information but all healthcare providers can be used as key champions for adult vaccination and work to improve health literacy and vaccine awareness in these communities.
Building community trust in these non-traditional vaccine pathways is a necessary step to ensuring the most effective usage, this can be done by training non-traditional vaccinators to be equipped to deal with vaccine hesitancy and skepticism, as well as leveraging trusted community leaders to support vaccination efforts within these communities. Individuals such as faith leaders, educators, and other leaders in their communities can provide valued insights into the needs of LMICs and identify potential barriers to vaccination that are community specific. Having buy-in from these leaders builds trust in the community and ensures that vaccine campaigns are robust and effective, while also provided the necessary care specific to each community.
This module explores opportunities to deliver vaccination campaigns in people-centered ways that include and specifically target older adults in low- and middle- income environments.
Relevant Resources:
- New immunization strategies: adapting to global challenges
- Building vaccine confidence and communicating vaccine value: toolkit
- COVID-19 Vaccination is Rising in Many Vulnerable African Communities Thanks to EU-funded, WHO-led Project
Learning Objectives:
- Describe how low- and middle- income settings experience additional burdens to vaccine supply, vaccine storage, and vaccine access.
- Identify examples of innovative practice that could be adapted and / or scaled in various communities.
- Highlight the ways that community buy-in and support from local leaders and trusted messengers contributes to vaccine campaign success.
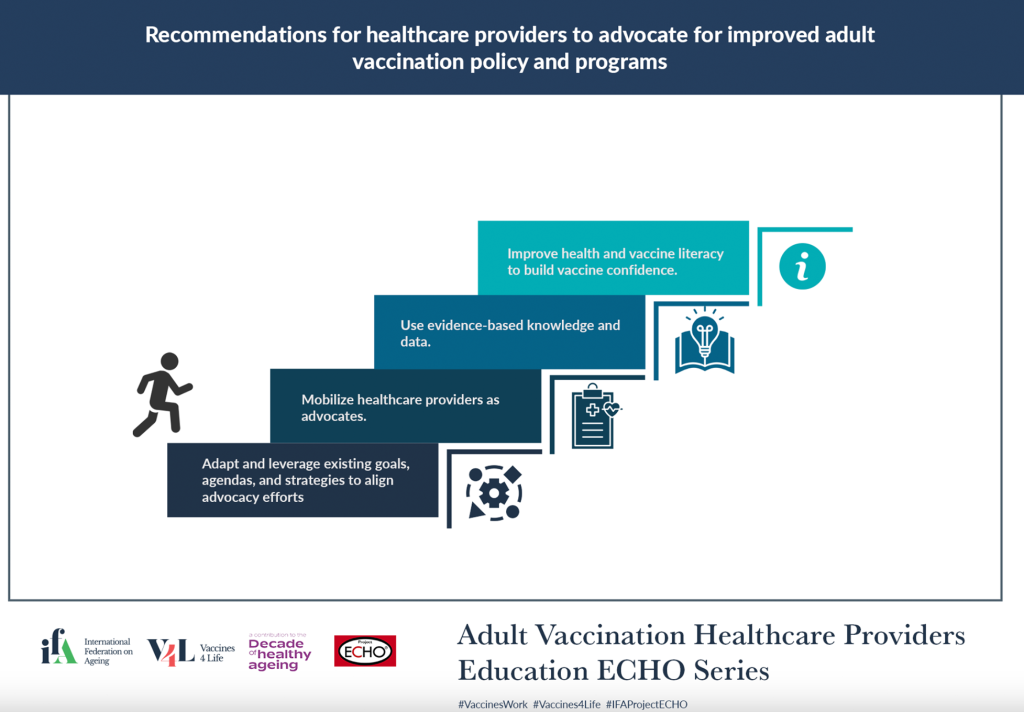
Healthcare providers as advocates for vaccination policy
Health care professionals (HCPs) remain one of the most trusted influencers in the realm of adult vaccination, not only as vaccinators of populations, but also as advocates to policymakers. This role can include publishing press releases urging government action, such as the Ontario Medical Association’s call to have all healthcare workers receive Covid-19 vaccines during the pandemic. However, policy change can also include working at the organizational level to ensure that there are comprehensive vaccination policies in place at workplaces, schools, etc.
Healthcare providers can influence policy due to their credibility as professionals, and experts in healthcare topics such as vaccination. They are also often invited to be on advisory committees or belong to professional organizations that have strong collective power and ability to campaign policymakers to drive change (6).
Examples of healthcare providers as advocates and drivers of policy change have been well-documented in other health related policies. In lobbying for health policy change, healthcare providers have been crucial in changing regulations around areas such as nicotine and tobacco usage. Learning from these past experiences and how they can be expanded to the role of healthcare providers in influencing adult vaccination policy is a key opportunity.
This module explores the important role of HCPs in calling for prioritization of older adults and availability of the appropriate infrastructure and resources to drive vaccine equity through policy change.
Relevant Resources:
Learning Objectives:
- Share current initiatives of healthcare providers and associations working to advocate for inclusive and equitable vaccination policies.
- Provide tangible strategies for increasing advocacy efforts of HCPs.
- Highlight key examples of HCPs changing health policy and explore how these can be extrapolated to the field of adult vaccination
Advisory Committee
Gonçalo Sousa Pinto
 Gonçalo Sousa Pinto, a pharmacist by background, leads the area of Development and Transformation of the pharmacy profession at the International Pharmaceutical Federation (FIP), the global organisation representing over 4 million pharmacists, pharmaceutical scientists and pharmaceutical educators. He supports the work of FIP member organisations and individual pharmacists around the world in advancing pharmacy practice and implementing pharmaceutical professional services in the areas of responsible use of medicines, in the prevention and management of non-communicable diseases as well as infectious diseases, including vaccination services.
Gonçalo Sousa Pinto, a pharmacist by background, leads the area of Development and Transformation of the pharmacy profession at the International Pharmaceutical Federation (FIP), the global organisation representing over 4 million pharmacists, pharmaceutical scientists and pharmaceutical educators. He supports the work of FIP member organisations and individual pharmacists around the world in advancing pharmacy practice and implementing pharmaceutical professional services in the areas of responsible use of medicines, in the prevention and management of non-communicable diseases as well as infectious diseases, including vaccination services.
He has authored or edited several publications to support and advocate a broader role by pharmacists in vaccination.
Ian DaSilva
 Ian DaSilva is Director of Operations of the Canadian Support Workers Association. Born in Toronto, Ian has extensive experience in working in the private, non-profit and governmental sectors in both strategic planning and policy development. Since 2018 Ian has worked with the Canadian Support Workers Association and the Ontario Personal Support Workers Association to oversee associations operations.
Ian DaSilva is Director of Operations of the Canadian Support Workers Association. Born in Toronto, Ian has extensive experience in working in the private, non-profit and governmental sectors in both strategic planning and policy development. Since 2018 Ian has worked with the Canadian Support Workers Association and the Ontario Personal Support Workers Association to oversee associations operations.
Ian holds a BA in Political Science and History from the University of Toronto and lives with his family in Whitby.
Stefania Maggi
 Stefania Maggi is a Geriatrician and Epidemiologist with specific interest in the epidemiology of aging and in the analysis of factors promoting healthy Aging in a lifelong approach. She is currently working as Research Director at the CNR Aging Branch-Institute of Neuroscience in Padua, Italy, and coordinating several national and international research projects on nutrition, vaccines and life style as key factors for promoting healthy aging.
Stefania Maggi is a Geriatrician and Epidemiologist with specific interest in the epidemiology of aging and in the analysis of factors promoting healthy Aging in a lifelong approach. She is currently working as Research Director at the CNR Aging Branch-Institute of Neuroscience in Padua, Italy, and coordinating several national and international research projects on nutrition, vaccines and life style as key factors for promoting healthy aging.
Dr. Maggi is past-President of the European Geriatric Medicine Society (EuGMS) and currently active in several EuGMS working groups, she is Vice-President of the European Interdisciplinary Council on Aging (EICA), member of the IOF Committee of Scientific Advisors and Member (ex-officio) of the ESCEO Board. Since 2016, she is a member of the Accademia Galileiana.
Steve Murigi
 Steve Murigi is a public health leader and advocate of inclusive, adaptive, localised and people-centred development practice, with extensive experience in international development across Africa and Europe. Over the years, he has worked across senior communication, advocacy, partnerships, and programme disciplines to drive organisational growth.
Steve Murigi is a public health leader and advocate of inclusive, adaptive, localised and people-centred development practice, with extensive experience in international development across Africa and Europe. Over the years, he has worked across senior communication, advocacy, partnerships, and programme disciplines to drive organisational growth.
Currently Head of Programmes and Strategic Partnerships at Amref Health Africa UK, Steve has a proven track record of mobilising resources and delivering high-worth, high-impact health programmes and partnerships, engaging civil society, private sector and government, to increase the breadth and depth of Amref Health Africa’s work.
Patricia M. D’Antonio
 Patricia M. D’Antonio, BSPharm, MS, MBA, BCGP is the Vice President of Policy and Professional Affairs for The Gerontological Society of America (GSA) and a board-certified geriatric pharmacist. Trish directs GSA’s policy initiatives and is responsible for developing relationships with organizations in the aging arena. Trish represents GSA on several policy coalitions and serves as co-chair for the Adult Vaccine Access Coalition, president of the board of the Protecting Access to Pain Relief and serves on the steering committee for several federally focused coalitions. Trish serves as the Executive Director for the National Center to Reframe Aging, the central hub to advance the long-term social change endeavor designed to improve the public’s understanding of what aging means and the many ways that older people contribute to our society. Additionally, Trish serves on the leadership team of the Resource Centers for Minority Aging Research National Coordinating Center. The national center provides support and coordination to the 18 resource centers and the National Institute on Aging to bolster the mentorship and career development of researchers from diverse backgrounds and foster rigorous behavioral and social science in aging, health disparities, equity, and Alzheimer’s Disease and Related Diseases.
Patricia M. D’Antonio, BSPharm, MS, MBA, BCGP is the Vice President of Policy and Professional Affairs for The Gerontological Society of America (GSA) and a board-certified geriatric pharmacist. Trish directs GSA’s policy initiatives and is responsible for developing relationships with organizations in the aging arena. Trish represents GSA on several policy coalitions and serves as co-chair for the Adult Vaccine Access Coalition, president of the board of the Protecting Access to Pain Relief and serves on the steering committee for several federally focused coalitions. Trish serves as the Executive Director for the National Center to Reframe Aging, the central hub to advance the long-term social change endeavor designed to improve the public’s understanding of what aging means and the many ways that older people contribute to our society. Additionally, Trish serves on the leadership team of the Resource Centers for Minority Aging Research National Coordinating Center. The national center provides support and coordination to the 18 resource centers and the National Institute on Aging to bolster the mentorship and career development of researchers from diverse backgrounds and foster rigorous behavioral and social science in aging, health disparities, equity, and Alzheimer’s Disease and Related Diseases.
Before joining GSA, Trish served as Executive Director for the District of Columbia Board of Pharmacy and Program Manager for the Pharmaceutical Control Division, where she was responsible for the regulatory and policy development for the practice of pharmacy and served as liaison to the FDA, DEA, and other federal, state, and city organizations that promote safe handling of medications. She received her Bachelor of Science in Pharmacy from Duquesne University and her Master of Science in Health Finance and Master in Business Administration with a concentration in health care from Temple University. She completed a residency in administration and finance at The Philadelphia Geriatric Center.
Afaayo Rachel Nakatugga
 Afaayo Rachel Nakatugga is a program Manager at East Africa Centre for Vaccines and Immunization (ECAVI). ECAVI is a not for profit initiative of health professionals, working with and through the Paediatric Associations, to promote Advocacy, Training, Research and Strengthening of immunization health systems in Eastern Africa to promote improved uptake and training on new and available vaccines; towards the control of morbidity and mortality associated with vaccine preventable diseases and cancers in Eastern Africa.
Afaayo Rachel Nakatugga is a program Manager at East Africa Centre for Vaccines and Immunization (ECAVI). ECAVI is a not for profit initiative of health professionals, working with and through the Paediatric Associations, to promote Advocacy, Training, Research and Strengthening of immunization health systems in Eastern Africa to promote improved uptake and training on new and available vaccines; towards the control of morbidity and mortality associated with vaccine preventable diseases and cancers in Eastern Africa.
Afaayo Rachel is a highly respected focal person for Immunization in Uganda and East Africa. She has served as an Immunization services Supervisor for different regions and districts during the immunization activities at Ministry of Health Uganda since 2015. She is a member of the immunization services delivery committee of Uganda. She holds a Master’s degree in Health Systems Management and is a trainer, researcher and advocate for immunization, with over 7 years’ experience of day to day interaction in immunization clinics. Afaayo Rachel is the coordinator of two highly sought-after annual courses; the Vaccinology Course for healthcare professionals, and the Resource Mobilization Course, both hosted by the ECAVI Vaccine Academy.
Kim Sampson
 Kim Sampson is CEO of the Australian Immunisation Coalition (since 2008), Executive Director of the Asia-Pacific Alliance for the Control of Influenza (APACI) since 2010, and President of the Australia-Vietnam Friendship Society (since 2013). Kim is a professional health administrator, commencing his career more than 35 years ago in Melbourne as the finance and laboratory manager at the Baker Medical Research Institute. His subsequent roles have included National Administration Manager for the Australian Brain Foundation, Business Manager at Southern Health Hospital Network, a Member of the Board of Monash Institute for Neurological Diseases, and General Manager at Neurosciences Australia.
Kim Sampson is CEO of the Australian Immunisation Coalition (since 2008), Executive Director of the Asia-Pacific Alliance for the Control of Influenza (APACI) since 2010, and President of the Australia-Vietnam Friendship Society (since 2013). Kim is a professional health administrator, commencing his career more than 35 years ago in Melbourne as the finance and laboratory manager at the Baker Medical Research Institute. His subsequent roles have included National Administration Manager for the Australian Brain Foundation, Business Manager at Southern Health Hospital Network, a Member of the Board of Monash Institute for Neurological Diseases, and General Manager at Neurosciences Australia.
He has been an educator for the Royal Australasian College of Surgeons’ training program and has co-authored a number of publications.
Dr Salah T. Al Awaidy
 Dr Salah Al Awaidy is a medical doctor, and holds a Masters in Epidemiology. His current position is Senior Consultant epidemiologist and Communicable Disease Surveillance and Control Adviser to the office of the Undersecretary of Health Affairs at the Ministry of Health, Oman. He currently advises on eradication, elimination and control of communicable diseases of public health importance, in addition to the Expanded Programme on Immunization (EPI), vaccine supply chain system and International Health Regulations.
Dr Salah Al Awaidy is a medical doctor, and holds a Masters in Epidemiology. His current position is Senior Consultant epidemiologist and Communicable Disease Surveillance and Control Adviser to the office of the Undersecretary of Health Affairs at the Ministry of Health, Oman. He currently advises on eradication, elimination and control of communicable diseases of public health importance, in addition to the Expanded Programme on Immunization (EPI), vaccine supply chain system and International Health Regulations.
He was Director-General of Communicable Diseases Control (CDC) between 1997-2002. In the national arena in the Ministry of Health, he played a pivotal role in reducing the national under-five mortality and morbidity, preparedness, management and control of infectious diseases such as SARS, avian influenza and pH1N1 and in establishing national communicable diseases, AEFI (Adverse Events Following Immunization) and rotavirus surveillance, as well as in the eradication of polio, measles, rubella, Congenital Rubella Syndrome (CRS) and leprosy in Oman. In addition, he played a fundamental role in reducing mortality and morbidity of vaccine-preventable diseases for paediatric, adolescent and adult populations in Oman.
Alia Alghwiri
 Alia Alghwiri a professor and founding chair of the department of physiotherapy at the Applied Science Private University in Jordan. She has been teaching for 12 years and became the first full professor in Jordan in 2019. Alia is a former president of the Jordanian Physiotherapy Society and the current general secretary of the Jordanian Athletic Therapy Association. She served as a member of congress programme committee for our congress in Geneva in 2019.
Alia Alghwiri a professor and founding chair of the department of physiotherapy at the Applied Science Private University in Jordan. She has been teaching for 12 years and became the first full professor in Jordan in 2019. Alia is a former president of the Jordanian Physiotherapy Society and the current general secretary of the Jordanian Athletic Therapy Association. She served as a member of congress programme committee for our congress in Geneva in 2019.
Her research interest focuses on the brain and how it affects physical and mental health. She has published around 40 articles and book chapters in the areas of vestibular disorders, multiple sclerosis, stroke, diabetes mellitus, ICF, and virtual reality. Alia has also been involved in two Erasmus plus projects in the areas of physiotherapy higher education and the issue of disability.
Alia has launched several initiatives and community programmes to raise awareness of the role of physiotherapy on disease prevention and physiotherapy management. These programmes have served people and refugees in the outskirts of Jordan, and benefited thousands of people who need medical advice and/or assistive devices.
Julia Tainijoki-Seyer
 Julia Tainijoki-Seyer is the Senior Advocacy and Medical Adviser of the World Medical Association. Dr Tainijoki-Seyer manages a variety of strategic projects at WMA ranging from infectious and noncommunicable diseases to strengthening health systems, patient safety, access to quality-assured medicines and the social determinants of health.
Julia Tainijoki-Seyer is the Senior Advocacy and Medical Adviser of the World Medical Association. Dr Tainijoki-Seyer manages a variety of strategic projects at WMA ranging from infectious and noncommunicable diseases to strengthening health systems, patient safety, access to quality-assured medicines and the social determinants of health.
Dr Tainijoki-Seyer serves as the WMA representative to the UN organizations, including WHO and other international institutions in Geneva, Switzerland. She also heads the secretariat of the World Health Professions Alliance (WHPA) representing more than 26 million healthcare professionals globally. Dr Tainijoki-Seyer is a family physician with a Master’s in International Health Economy and Policy from the University of Bocconi in Milan, Italy.
Prof Joseph Ana
 Prof Joseph Ana is the Lead Senior Fellow and Medical Consultant at the Centre for Clinical Governance Research and Patient Safety (CCGR&PS) established by HRI Global (former HRIWA) with Headquarters in Calabar, Nigeria. www.hri-global.org He is the Country Coordinator for ‘PACK Nigeria’ (Practical Approach to Care Kit which is specifically developed to improve clinical competence -improving accuracy of diagnosis and treatment – in primary health care. He is a Member of the World Health Organisation’s Technical Advisory Group on Integrated Care in primary, emergency, operative, and critical care (TAG-IC2). As the Cross River State Commissioner for Health (2004-2008), Joseph Ana led the design, development and pilot of the 12-Pillar Clinical Governance Programme (12-PCGP) in Nigeria, in 2004, as a whole health sector and system approach to transforming failing health systems in lower-, low-, and middle income countries (LLMIC). It is a context focused, evidence based and homegrown quality tool.
Prof Joseph Ana is the Lead Senior Fellow and Medical Consultant at the Centre for Clinical Governance Research and Patient Safety (CCGR&PS) established by HRI Global (former HRIWA) with Headquarters in Calabar, Nigeria. www.hri-global.org He is the Country Coordinator for ‘PACK Nigeria’ (Practical Approach to Care Kit which is specifically developed to improve clinical competence -improving accuracy of diagnosis and treatment – in primary health care. He is a Member of the World Health Organisation’s Technical Advisory Group on Integrated Care in primary, emergency, operative, and critical care (TAG-IC2). As the Cross River State Commissioner for Health (2004-2008), Joseph Ana led the design, development and pilot of the 12-Pillar Clinical Governance Programme (12-PCGP) in Nigeria, in 2004, as a whole health sector and system approach to transforming failing health systems in lower-, low-, and middle income countries (LLMIC). It is a context focused, evidence based and homegrown quality tool.
To ensure sustainability of the 12-PCGP, he established the ‘Department of Clinical Governance, Servicom & e-health’ in the Cross River State Ministry of Health in 2007. In 2009, he was promoted to Adjunct Professor in the Faculty of Health Sciences of the Cross River University of Technology, Nigeria.
Hub Team
Ian DaSilva
 Ian DaSilva is Director of Operations of the Canadian Support Workers Association. Born in Toronto, Ian has extensive experience in working in the private, non-profit and governmental sectors in both strategic planning and policy development. Since 2018 Ian has worked with the Canadian Support Workers Association and the Ontario Personal Support Workers Association to oversee associations operations.
Ian DaSilva is Director of Operations of the Canadian Support Workers Association. Born in Toronto, Ian has extensive experience in working in the private, non-profit and governmental sectors in both strategic planning and policy development. Since 2018 Ian has worked with the Canadian Support Workers Association and the Ontario Personal Support Workers Association to oversee associations operations.
Ian holds a BA in Political Science and History from the University of Toronto and lives with his family in Whitby.
Prof Joseph Ana
 Prof Joseph Ana is the Lead Senior Fellow and Medical Consultant at the Centre for Clinical Governance Research and Patient Safety (CCGR&PS) established by HRI Global (former HRIWA) with Headquarters in Calabar, Nigeria. www.hri-global.org He is the Country Coordinator for ‘PACK Nigeria’ (Practical Approach to Care Kit which is specifically developed to improve clinical competence -improving accuracy of diagnosis and treatment – in primary health care. He is a Member of the World Health Organisation’s Technical Advisory Group on Integrated Care in primary, emergency, operative, and critical care (TAG-IC2). As the Cross River State Commissioner for Health (2004-2008), Joseph Ana led the design, development and pilot of the 12-Pillar Clinical Governance Programme (12-PCGP) in Nigeria, in 2004, as a whole health sector and system approach to transforming failing health systems in lower-, low-, and middle income countries (LLMIC). It is a context focused, evidence based and homegrown quality tool.
Prof Joseph Ana is the Lead Senior Fellow and Medical Consultant at the Centre for Clinical Governance Research and Patient Safety (CCGR&PS) established by HRI Global (former HRIWA) with Headquarters in Calabar, Nigeria. www.hri-global.org He is the Country Coordinator for ‘PACK Nigeria’ (Practical Approach to Care Kit which is specifically developed to improve clinical competence -improving accuracy of diagnosis and treatment – in primary health care. He is a Member of the World Health Organisation’s Technical Advisory Group on Integrated Care in primary, emergency, operative, and critical care (TAG-IC2). As the Cross River State Commissioner for Health (2004-2008), Joseph Ana led the design, development and pilot of the 12-Pillar Clinical Governance Programme (12-PCGP) in Nigeria, in 2004, as a whole health sector and system approach to transforming failing health systems in lower-, low-, and middle income countries (LLMIC). It is a context focused, evidence based and homegrown quality tool.
To ensure sustainability of the 12-PCGP, he established the ‘Department of Clinical Governance, Servicom & e-health’ in the Cross River State Ministry of Health in 2007. In 2009, he was promoted to Adjunct Professor in the Faculty of Health Sciences of the Cross River University of Technology, Nigeria.
Jia Hu
 Jia Hu is a family physician and public health and preventive medicine specialist. He is currently the CEO of 19 To Zero, a not-for-profit focused on public health behaviour change such as increasing vaccination rates or cancer screening rates. He is also an adjunct professor at the University of Calgary and a medical director with Cleveland Clinic Canada where he advises large companies on health and wellness topics ranging from pandemic preparedness to mental health and preventative health. He is on the board of the international health NGO, Partners in Health Canada and is an adjunct professor at the University of Calgary.
Jia Hu is a family physician and public health and preventive medicine specialist. He is currently the CEO of 19 To Zero, a not-for-profit focused on public health behaviour change such as increasing vaccination rates or cancer screening rates. He is also an adjunct professor at the University of Calgary and a medical director with Cleveland Clinic Canada where he advises large companies on health and wellness topics ranging from pandemic preparedness to mental health and preventative health. He is on the board of the international health NGO, Partners in Health Canada and is an adjunct professor at the University of Calgary.
He previously worked as a medical officer of health with Alberta Health Services and worked in management consulting with McKinsey & Co.
Dr Edina Amponsah-Dacosta
 Dr Edina Amponsah-Dacosta is a trained Medical Virologist, Vaccinologist and Health Systems researcher. She has an MSc and PhD in Medical Virology from the Sefako Makgatho Health Sciences University, South Africa, and an MPH (Health Policy and Systems specialization) from the University of Cape Town (UCT), South Africa. She also completed a five-year Postdoctoral Research Fellowship in Vaccinology with the Vaccines for Africa Initiative (VACFA), also based at UCT.
Dr Edina Amponsah-Dacosta is a trained Medical Virologist, Vaccinologist and Health Systems researcher. She has an MSc and PhD in Medical Virology from the Sefako Makgatho Health Sciences University, South Africa, and an MPH (Health Policy and Systems specialization) from the University of Cape Town (UCT), South Africa. She also completed a five-year Postdoctoral Research Fellowship in Vaccinology with the Vaccines for Africa Initiative (VACFA), also based at UCT.
As a Research Officer and Evidence-Informed Decision-Making Specialist (EIDM) at VACFA, Edina is involved in strengthening expert recommendations on vaccines and immunization services in Africa. To this end, she is involved in the development of EIDM resources, Vaccinology and EIDM courses and capacity development workshops geared towards members of National Immunization Technical Advisory Groups (NITAGs). This work forms part of the NITAG Support Hub (NISH) project which is underwritten by the World Health Organization and made possible with funding from The Wellcome Trust. In line with VACFA’s vision of “An Africa free of vaccine preventable diseases”, Edina’s research focus draws on her strong interdisciplinary expertise in pursuing the goal of expanding the reach of lifesaving vaccines and reducing the burden of vaccine preventable diseases across the African region. She is the Principal Investigator of a Gilead Sciences sponsored project assessing the neglected burden of viral hepatitis among HIV-exposed uninfected and infected pediatric populations. She is also interested in scaling-up health systems capacity to support under-utilized immunization programmes like hepatitis B birth-dose vaccination, Human Papillomavirus vaccination, and maternal immunization programmes. Edina is also involved in conducting clinical trials and systematic reviews, postgraduate teaching and supervision, and co-organizes the Annual African Vaccinology Course hosted by VACFA. She is an affiliate member of the African Academy of Sciences.
Dr. Lulu C. Bravo
 Dr. Lulu C. Bravo is a professor emeritus at the College of Medicine at the University of the Philippines Manila. She is also the former vice chancellor for Research and Executive Director of the National Institutes of Health. She is the current president of the Immunization Partners in Asia Pacific (IPAP) and the founding president of the Philippine Foundation for Vaccination.
Dr. Lulu C. Bravo is a professor emeritus at the College of Medicine at the University of the Philippines Manila. She is also the former vice chancellor for Research and Executive Director of the National Institutes of Health. She is the current president of the Immunization Partners in Asia Pacific (IPAP) and the founding president of the Philippine Foundation for Vaccination.
In 2018 she was awarded the Outstanding Professional in Medicine Award given by the Professional regulation Commission of the Philippines. She has also been awarded the 2012 Asian Outstanding Pediatrician and 2011 Dr. Jose Rizal Memorial Award for Academe.